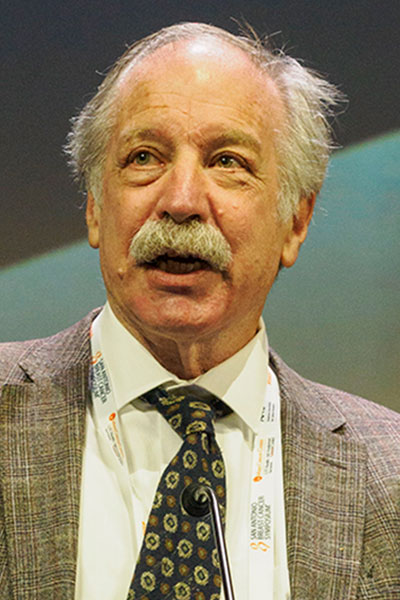
The 2023 William L. McGuire Memorial Lecture Award was given to Jack Cuzick, PhD, for his pioneering work in breast cancer prevention. He presented his lecture, Progress on the Prevention of Breast Cancer, on Wednesday, December 6.
The session is available on demand for registered 2023 SABCS® participants through March 31, 2024, on the meeting platform.
“Prevention is the way forward,” said Dr. Cuzick, John Snow Professor of Epidemiology at Queen Mary University of London, United Kingdom. “We need to think more like cardiologists. They don’t wait for someone to get a heart attack to treat them. Breast cancer is a great place to start thinking about prevention in oncology because we have a lot of evidence to support it.”
Dr. Cuzick identified the role of tamoxifen in preventing contralateral breast cancer nearly 40 years ago in the NATO trial. This provided the rationale for larger, confirmatory trials of tamoxifen and other agents in breast cancer prevention.
Getting these trials off the ground, however, was not easy. Dr. Cuzick noted that people were worried about the potential side effects of tamoxifen and the need for long-term investment.
“Prevention is a long-term game.” Dr. Cuzick said. “If you stop a trial too early, you will miss some major important findings. You need to be looking at a 20-year follow-up.”
The importance of long-term follow-up was demonstrated in IBIS-I, a study comparing the impact of five years of tamoxifen with that of placebo in more than 7,000 women at high risk of breast cancer.
At 10 years of follow-up, the cumulative incidence of breast cancer was 6.3% in the placebo group and 4.6% in the tamoxifen group. At 20 years, the gap had widened: Cumulative incidence of breast cancer was 12.3% in the placebo group and 7.8% in the tamoxifen group.
“Even though you stop treatment at five years, the benefits in years 10-20 were bigger than in the first 10 years,” said Dr. Cuzick. “There’s something about tamoxifen that gives you long, lifetime prevention.”
Similar effects have been seen with raloxifene and aromatase inhibitors.
Given that no therapy is without risk, identifying who is most likely to benefit from prophylactic treatments is important to spare patients from unwarranted side effects. Dr. Cuzick showed that estrogen levels may provide some insight into who is most likely to benefit from aromatase inhibitors using data from the IBIS-II trial.
“Estrogen is one of the strongest risk factors for breast cancer but is rarely measured,” he said. “There’s evidence that this needs to change.”
In women at high risk of breast cancer who received anastrozole, those with high estradiol levels experienced a 50% reduction in new cancers compared to the placebo group. In contrast, there was essentially no benefit of anastrozole in those with low estradiol levels.
“There is very little benefit in women with low estradiol,” said Dr. Cuzick. “We need to pay attention to this, and potentially change how we manage breast cancer. Measuring estradiol may improve the risk-benefit of anastrozole. We can select which patients are most likely to benefit and spare patients who won’t benefit from the side effects of this drug.”

