Wednesday morning’s General Session 2 featured findings from three trials looking at the use of the antibody drug conjugate (ADC) trastuzumab deruxtecan (T-DXd) in HER2-positive metastatic and HER-2-low, HR-positive early-stage breast cancer.
GS2-01: Trastuzumab deruxtecan vs physician’s choice in patients with HER2+ unresectable and/or metastatic breast cancer previously treated with trastuzumab emtansine: primary results of the randomized, phase 3 study DESTINY-Breast02
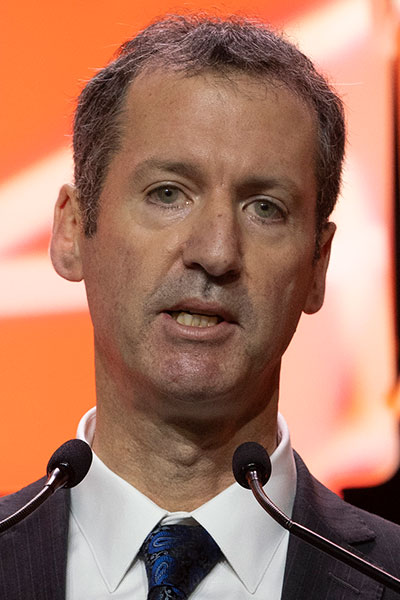
Ian Krop, MD, PhD, Associate Cancer Center Director for Clinical Research and the chief clinical research officer at the Yale Cancer Center, presented the latest findings from the phase III DESTINY-Breast02 trial which demonstrated that trastuzumab deruxtecan (T-DXd), when compared with capecitabine + lapatinib or capecitabine + trastuzumab, led to higher response rates and longer survival in the third-line setting for patients with HER2-positive metastatic breast cancer previously treated with trastuzumab emtansine (T-DM1).
In the single-arm DESTINY-Breast01 phase II clinical trial, T-DXd showed clinical activity in the third-line setting for patients with HER2-positive metastatic breast cancer who were previously treated with T-DM1. These results led to the accelerated approval of T-DXd in 2019 as a third-line therapy for patients with metastatic or unresectable breast cancer who have received two or more prior HER2-targeted therapies.
“While DESTINY-Breast01 established T-DXd as a new treatment for this population, it was a modestly sized, single-arm phase II trial,” Dr. Krop said.
The DESTINY-Breast02 trial was designed as a confirmatory study for DESTINY-Breast01 to evaluate T-DXd versus treatment of physician’s choice (TPC) in patients previously treated with T-DM1, he noted.
DESTINY-Breast02 enrolled 608 patients whose metastatic breast cancers had progressed on or after T-DM1 treatment. Patients were randomly assigned 2:1 to receive either T-DXd or TPC (a combination of capecitabine with either trastuzumab or lapatinib).
Among the patients treated with T-DXd, 69.7% experienced an objective response, as compared with 29.2% of patients treated with TPC. Those treated with T-DXd were also 64% less likely to experience disease progression than patients receiving TPC, with a median progression-free survival of 17.8 months and 6.9 months for patients in the T-DXd and TPC arms, respectively. Overall survival was also significantly longer for patients treated with T-DXd (39.2 months with T-DXd vs. 26.5 months with TPC).
“The results of DESTINY-Breast02 confirm the findings of DESTINY-Breast01, demonstrating high levels of efficacy of T-DXd in patients with HER2-positive metastatic breast cancer previously treated with T-DM1,” Dr. Krop said. “Furthermore, they extend these findings, demonstrating that T-DXd is not only highly active, but also superior to conventional chemotherapy-based regimens in this patient population.”

GS2-02: Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: Updated survival results of the randomized, phase 3 study DESTINY-Breast03
Sara Hurvitz, MD, Professor of Medicine at the David Geffen School of Medicine at the University of California Los Angeles and Jonsson Comprehensive Cancer Center, reported updated results from the DESTINY-Breast03, a phase III clinical trial of second-line treatment with T-DXd.
The DESTINY-Breast03 trial compared the efficacy and safety of T-DXd with those of T-DM1 in patients with HER2-positive metastatic breast cancer that progressed on or after first-line treatment. Previously published interim results from the trial demonstrated that patients treated with T-DXd had significantly longer progression-free survival (PFS) compared with patients who received T-DM1. These results led to the approval of T-DXd as a second-line treatment for this patient population. However, overall survival data had not been reached in the first interim analysis, Dr. Hurvitz said.
In DESTINY-Breast03, 524 participants with HER2-positive unresectable or metastatic breast cancer previously treated with trastuzumab plus chemotherapy were randomly assigned to receive either T-DXd or T-DM1. Participants assigned to the T-DXd arm had longer time without progression of their cancer and also had longer survival time compared to participants assigned to the T-DM1 arm. Similar proportions of participants experienced side effects across the two groups, Dr. Hurvitz reported, noting that T-DXd treatment showed side effects consistent with earlier T-DXd studies.
“The results of this analysis demonstrated remarkable overall survival and continued PFS benefit with T-DXd in patients with HER2-positive metastatic breast cancer who progressed on prior therapy, further supporting the use of T-DXd over T-DM1 in the second-line setting,” said Dr. Hurvitz. “With this overall survival analysis, we can confirm that the previously demonstrated benefit from T-DXd in PFS improvement transforms into a statistically significant improvement in overall survival, a substantial advantage for our patients.”

GS2-03: TRIO-US B-12 TALENT: Neoadjuvant trastuzumab deruxtecan with or without anastrozole for HER2-low, HR+ early stage breast cancer
Aditya Bardia, MD, MPH, Attending Physician at Mass General Cancer Center and Director of Breast Cancer Research and Associate Professor at Harvard Medical School, presented results from the phase II TRIO-US B-12 TALENT trial demonstrating that patients with localized, HR-positive, HER2-low breast cancer treated with T-DXd in the neoadjuvant setting had an overall response rate of 75% in the absence of anastrozole and 63% in combination with anastrozole.
“This is the first report of neoadjuvant T-DXd for patients with HR-positive, HER2-low, localized breast cancer,” Dr. Bardia said. “It could provide the groundwork for future studies with antibody-drug conjugates, including T-DXd, for patients with early-stage breast cancer.”
This phase II investigator-initiated clinical trial was designed to evaluate efficacy of T-DXd in patients with localized HR-positive/HER2-low breast cancer.
“Given the cross-talk between ER and HER2, we also evaluated whether addition of endocrine therapy would improve efficacy of T-DXd in this setting,” Dr. Bardia said.
The primary endpoint for the study was a 5% pathologic complete response (pCR) rate, defined as complete tumor regression and no lymph node involvement at the time of surgery.
At the time of first data cutoff, Dr. Bardia reported that no patients had experienced a pCR in the combination treatment arm, and one out of 19 patients (5.3%) had experienced a pCR in the solo treatment arm.
As of the data cutoff, 33 patients had completed neoadjuvant treatment and undergone surgery, seven patients were awaiting surgery, and 13 patients were still undergoing T-DXd treatment. Among the response-evaluable population, in the solo treatment arm, the overall response rate was 75%, including 11 partial responses and one complete response. In the combination treatment arm, the overall response rate was 63%, including 10 partial responses and two complete responses.
“The study demonstrated that T-DXd was relatively safe in HER2-low, HR-positive, localized breast cancer. It provides a translational framework for future studies, including combination regimens in the neoadjuvant setting to further improve clinical outcomes,” Dr. Bardia said.
On-Demand Session Availability
Daily sessions will be available for on-demand viewing 3-5 days following the 2022 Symposium (author permitting). They will be available exclusively to registered SABCS attendees until March 2023. Following March 2023, they will be available on SABCS.org under the “Resources” tab.

