A panel of experts conveyed state-of-the-art concepts in the understanding of tumor heterogeneity, evolution, and drug resistance during the Basic Science Workshop on Tuesday, the first day of the 2022 San Antonio Breast Cancer Symposium.
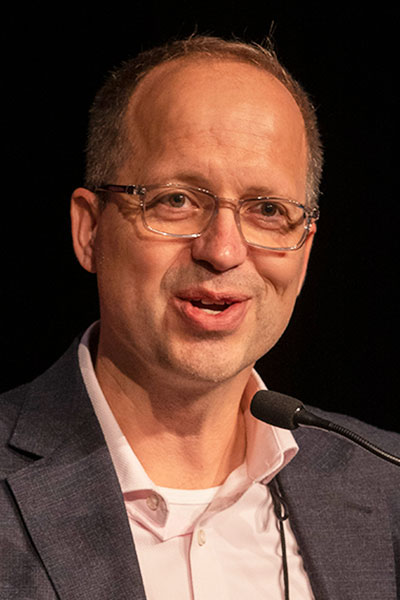
Reuben Harris, PhD, Professor and Chair of Biochemistry and Structural Biology, The University of Texas Health Science Center at San Antonio, opened the workshop with a focus on the APOBEC (apolipoprotein B mRNA editing enzyme catalytic polypeptide) protein family and its effects on genome evolution in metastatic breast cancer.
APOBEC plays important roles in the development of multiple cancer types, most often through overexpression. Two APOBEC proteins, A3A and A3B, are particularly active in breast cancers.
“High APOBEC levels in the primary tumor predict poor outcomes following recurrence,” Dr. Harris said. “APOBEC is an important and spontaneous driver of mutations in breast cancer that is capable of degrading the genome and inflicting widespread damage.”
APOBEC activity can be identified using characteristic DNA substitution signatures. In breast cancer, the signature C-to-T substitution appears to underlie both tumorigenesis and tumor evolution.
“I think of APOBEC as an enabler, the fuel that drives genomic changes leading to cancer,” Dr. Harris said.
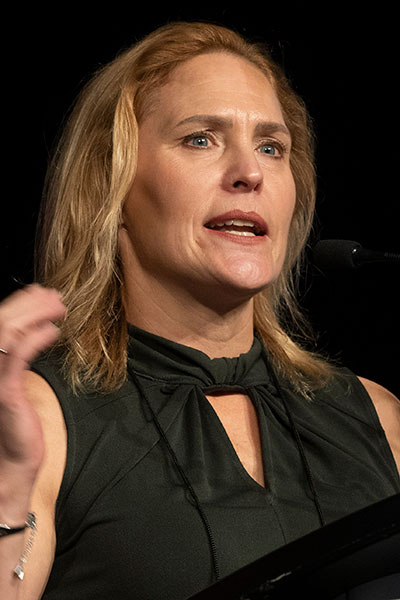
Age is another key driver of cancer. Multiple cancer types begin to surge around the age of 50 to 60, noted Sheila Stewart, PhD, Gerty Cori Professor of Cell Biology & Physiology, Washington University School of Medicine, who spoke about therapy-induced senescence.
“Most adult cancers are the result of multiple mutations over many years,” Dr. Stewart said. “It takes time to accumulate enough mutations and the right order of mutations to develop cancer. Senescent fibroblasts promote tumorigenesis and increase tumor cell proliferation, migration, invasion, angiogenesis and immunosuppressive cells just like cancer-associated fibroblasts.”
Selective elimination of senescent cells delays the development of tumors in mouse models. In primary tumors, the p38MAPK-MK2 pathway supports tumor growth, while inhibiting p38 limits the pro-tumorigenic potential of senescent fibroblasts. Similarly, p38MAPK-dependent factors are expressed in the stromal compartment of metastatic breast cancer lesions in bone, while inhibiting p38MAPK decreases both visceral and bone metastases.
In mouse models, p38/MK2 inhibition is as effective as paclitaxel in limiting tumor growth, Dr. Stewart said. More importantly, mice treated with p38/MK2 inhibition are more mobile and more active than mice treated with paclitaxel. Inhibiting p38MAPK-MK2 reduces bone metastasis and preserves bone integrity, an effect not seen with chemotherapy agents that typically lead to bone loss.
“If we see success in the metastatic setting, maybe it will be possible to help our patients live better as well as live longer,” Dr. Stewart said.

Cancer therapy resistance is another promising therapeutic target. Until recently, therapy resistance has focused largely on genetic alterations and Darwinian selection processes.
“Clinical and experimental evidence is emerging for the existence of non-genetic mechanisms for drug tolerance,” said Joan S. Brugge, PhD, Louise Foote Pfeiffer Professor of Cell Biology and Director of the Ludwig Center, Harvard Medical School. “Cancer therapies can induce transient drug-tolerant cell states before the development of stable genetic resistance. These drug-tolerant persister (DTP) cells represent an untouched therapeutic opportunity.”
Tumor cells can exhibit multiple types of adaptive, non-genetic changes that allow them to survive treatment, Dr. Brugge continued. Single-cell RNA sequencing and barcode lineage tracing have shown that most tumor cells have an equipotent capacity to enter a DTP state that is stable for multiple divisions. Tumors that recur following a DTP state maintain clonal complexity and treatment sensitivity that is similar to the primary tumor.

“We need a better understanding of the cellular programs required for survival of DTPs and effective pharmacologic inhibitors of the adaptive response and DTP programs,” Dr. Brugge said. “We need tumor-targeting formulation and combinations that are systemically toxic and integrate them with immunotherapy.”
DNA replication timing is another potential target. DNA replication occurs at specific times during the cell cycle, explained Nnenna Kanu, PhD, Principal Research Fellow, University College London Cancer Institute.
Replication timing late in the cell cycle is associated with lower levels of DNA repair, increased DNA damage, and greater mutation density. Alterations in replication timing, particularly a shift from early replication to late replication, are similarly associated with a sharp increase in mutation load.
“Alterations in replication timing are likely an early event in breast cancer evolution,” Dr. Kanu said. “We can now identify altered replication timing at single cell resolution.”
On-Demand Session Availability
Daily sessions will be available for on-demand viewing 3-5 days following the 2022 Symposium (author permitting). They will be available exclusively to registered SABCS attendees until March 2023. Following March 2023, they will be available on SABCS.org under the “Resources” tab.

