The intrinsic subtypes and immune signatures of breast cancer contribute to a variety of factors, including baseline prognosis, prognosis for ER-positive and endocrine therapy-treated patients, and prediction of response to CDK4/6 inhibitors, HER2-targeting, chemotherapy, and immune checkpoint inhibitors.
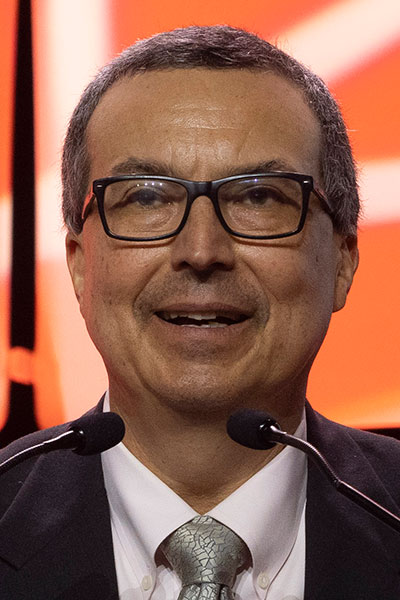
“Quantitative and objective means of measuring both is important,” said Charles M. Perou, PhD, in the 2022 AACR Distinguished Lectureship in Breast Cancer Research on Wednesday, December 7. “I’m also going to argue that we can come up with methods that put them together into multifactor models that can give us risk scores, and then we can draw cutoffs for clinical use.”
This lectureship is an award that recognizes outstanding science that has inspired—or has the potential to inspire—new perspectives on the etiology, diagnosis, treatment, or prevention of breast cancer. A pioneer in cancer genomics research, Dr. Perou is Professor in the Department of Genetics and the Co-director of the Computational Medicine Program at the University of North Carolina at Chapel Hill, Faculty Director of the Lineberger Comprehensive Cancer Center (LCCC) Bioinformatics Group, and Co-director of the LCCC Breast Cancer Research Program.
Beyond the three clinical subtypes of breast cancer (hormone receptor positive/ HER2-negative, triple-negative, and HER2-positive), the disease can be stratified into intrinsic subtypes: luminal A and B, basal-like, and HER2-enriched.
“Every clinical subtype has all intrinsic subtypes in it,” Dr. Perou said. “The numbers get vastly skewed one way or another. In ER-positives and HER2-negatives, it’s largely luminal. In triple-negatives, it’s largely the basal-like type.”
Within a 2019 study sample, 89 percent of HR-positive/HER2-negative patients were in the luminal A and B subtype. Among triple-negative patients, 78 percent were in the basal-like subtype. HER2-positive disease appears to be the most heterogeneous disease in breast cancer, Dr. Perou noted.
“You’ve got all the subtypes there at significant proportions, and I think this explains some of the behavior and differences in outcomes we see in HER2-positive disease,” he said.
There is a notable disconnect when comparing event-free survival (EFS) outcomes by intrinsic subtype. HER2-enriched patients, despite having the best pathological complete response (pCR) rate, have a lower survival rate compared to the luminal A subtype which has the lowest pCR rate but the best survival rate.
“We need to keep that in mind as we design these trials for patients who have residual disease, many of whom are luminal A type and endocrine therapy is going to be the mainstay of those patients and likely why they have such a good outcome,” he said.
Among triple-negative patients, the intrinsic subtype of disease has not shown to be predictive of survival, yet it does factor into the tumor-immune microenvironment, Dr. Perou noted.
“In triple-negative disease, I’m going to say knowing your immune type is really important, particularly the presence of B cells and T cells,” he said.
In HER2-positive disease, both the intrinsic subtype and immune type affect survival rates.
Survival, pathologic response, and genomics in the CALGB 40601 data showed all significant immune signatures are strongly correlated with higher pCR rates and longer EFS, Dr. Perou noted.
“[This] highlights the importance of the immune system, where high expression of particularly B cell, the IgG (immunoglobulin) signature, and T cell signature predicts both a better response and a better survival,” he said. This discovery contributed to the development of the HER2DX assay for predicting pathological response and survival outcomes in early-stage HER2-positive breast cancer.

